For some patients with multiple sclerosis (MS), a bone marrow or blood stem cell transplant has shown to be a successful, if dangerous, therapy option. Now, researchers have a better understanding of how and why this treatment might suppress autoimmunity and restore immunological function. With a deeper understanding of the method’s theoretical underpinnings, it would be possible to expand access to it beyond its current geographical scope. Science Translational Medicine has published the results.
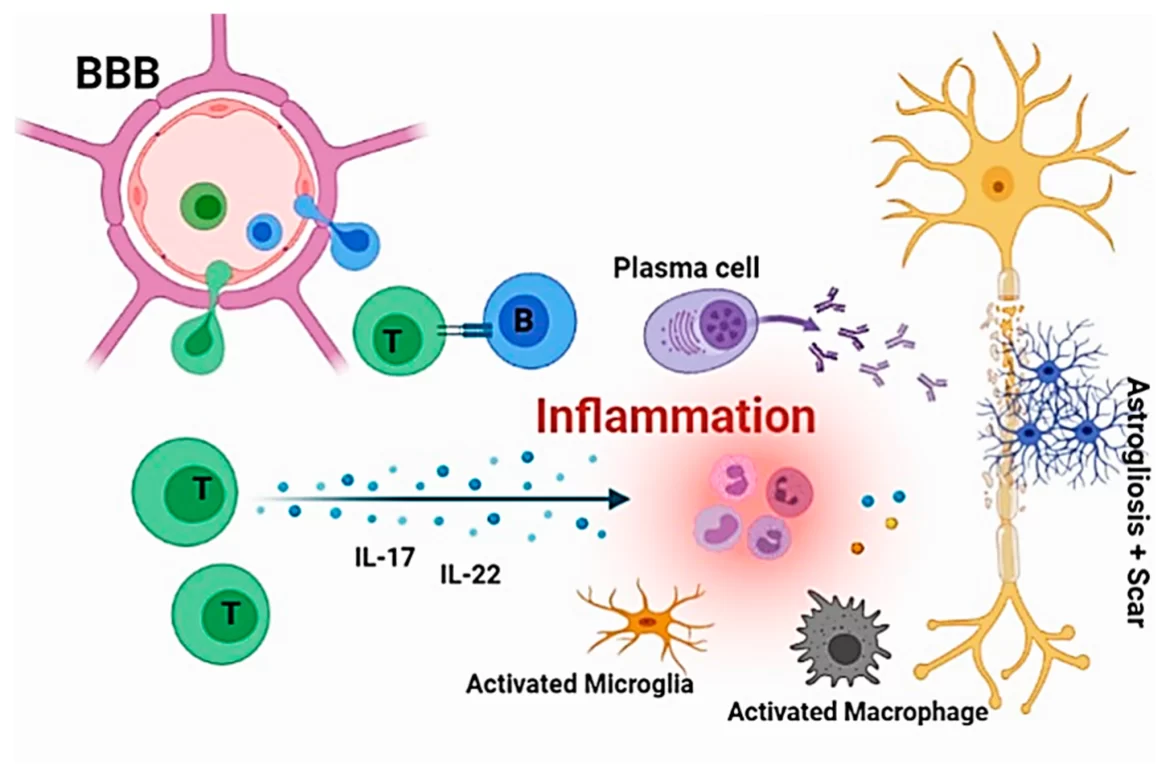
Myelin sheath disease is a disorder in which the body’s immune system mistakenly targets the protective covering of nerve cells. Some of the most disabling symptoms of this disease come from the damage done to neurons in the central nervous system, and these include extreme tiredness, pain, and even paralysis.
Professor Roland Martin of the University of Zurich, who just resigned as the study’s senior author, said that eighty percent of MS patients who get an autologous hematopoietic stem cell transplant are cured of the condition permanently.
The transplant therapy is more effective for younger patients with more severe types of MS. This very successful and low-mortality therapy is exclusively available at the clinic at Switzerland’s University Hospital Zurich (USZ).
There may be adverse effects from the therapy. As a first step, a patient’s bone marrow is extracted for its stem cells’ ability to produce new immune cells in the blood. The next step is to use a combination of chemotherapy medications to completely wipe out the immune system, eliminating the cells in the bone marrow responsible for making immune cells like the T cells responsible for attacking the central nervous system in MS. After removing the autoreactive cells that target the myelin sheath of neurons, the patient’s blood stem cells are reintroduced. This allows the body to renew its immune system.
This research clarified a number of issues, including whether or not the return of autoimmune cells and the survival of any immune cells at all was to be expected following chemotherapy.
Researchers looked at 27 MS patients before, during, and up to two years following the treatment. In spite of surviving chemotherapy, memory T cells, which quickly resurfaced after the transplant and reactivate when exposed to a reactivated infection, were a major disappointment. It is not believed that they increase the likelihood of a relapse in multiple sclerosis.
“They are pre-damaged owing to the treatment and consequently no longer able to generate an autoimmune response,” said Martin.
In the months after the treatment, the thymus played a pivotal role in the progressive regeneration of several immune cell types.
“Adults have very little working tissue remaining in the thymus, but following a transplant, the organ seems to restart its activity and assures the formation of a whole new repertoire of T cells that plainly do not trigger MS or cause it to recur,” said Martin.
However, more, costly Phase III studies probably won’t be necessary to make this medicine available in other nations.
Pharmaceutical corporations are only interested in funding Phase III research, which may cost several hundred million euros, if they can expect to earn money off of them, as noted by Martin. Stem cell therapies don’t make use of patented pharmaceuticals, hence they don’t provide long-term financial gain.
In order to get this therapy, some people with MS have traveled to Israel or Mexico. Eventually, I hope that this possible solution will be available to a wider range of people.
Data from the University of Zurich and Science Translational Medicine.